What are Biofilms?
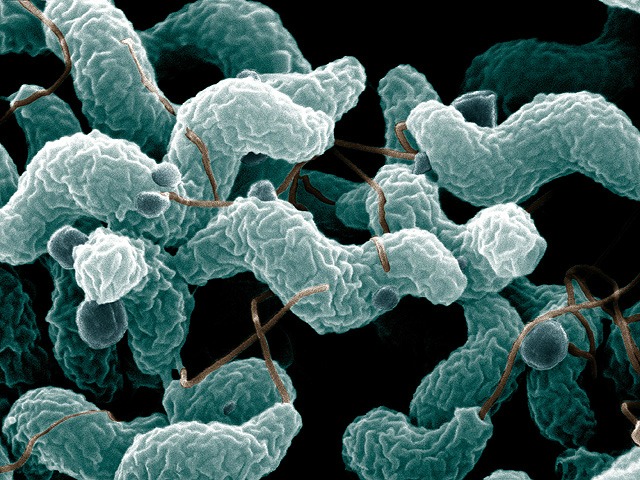
Biofilm consists of microorganisms encased within a self-produced matrix of exopolysaccharides and exoproteins that strongly adheres to interfaces and resists dislodgement. Microorganisms residing within biofilms are highly resistant to antimicrobials including antibiotics and bacteriocins produced by probiotics.
Biofilm Protects Potential Pathogens from Predation
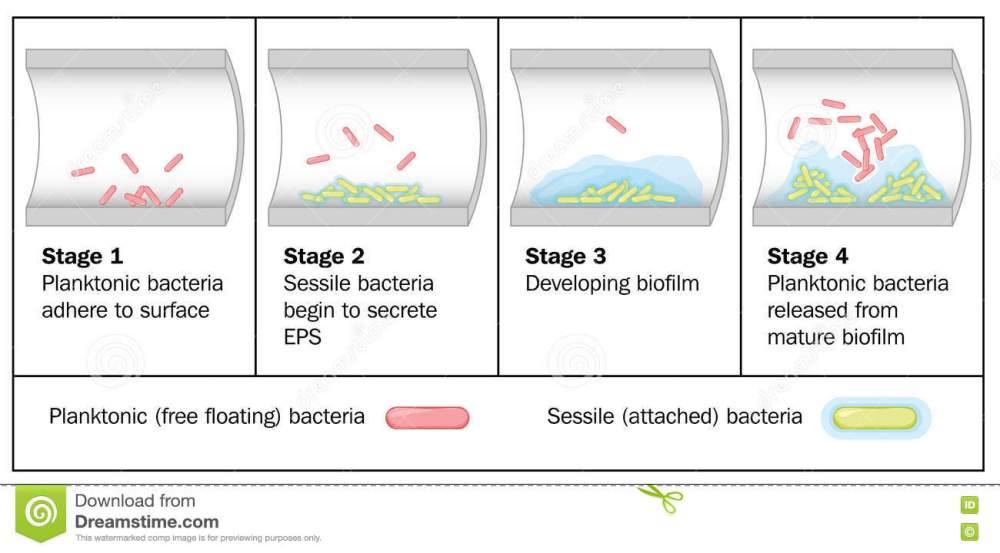
Biofilm is the preferred form of life for the vast majority of microorganisms. Microbes residing within biofilms may consist of one or more species that communicate and collaborate with one another in a heterogeneous community. Biofilm formation appears to be initiated by contact with a surface. It is a survival mechanism that triggers downregulation of genes such as those mediating motility and growth as well as expression of genes regulating synthesis of exopolysaccharides and exoproteins. The presence of calcium, iron, and magnesium is essential for biofilm creation and serves to cross-link the anionic regions of polymers. Life within a biofilm confers significant survival advantages to bacteria and yeasts. Biofilms strongly adhere to interfaces and resist dislodgement. Biofilm formation may be viewed as an adaptive mechanism that enables microbes to persist and reproduce in an advantageous microecological niche. They are protected from predation by phages and protozoa as well as from host immune responses. Biofilm-residing microorganisms are highly resistant to the spectrum of antimicrobials ranging from germicides and disinfectants to antibiotics and bacteriocins produced by probiotics. Sessile biofilm microorganisms are 100 to 1000 times more resistant to antibiotics compared to planktonic forms of the same strain. Antibiotic resistance of biofilm-associated organisms has been attributed to impaired antimicrobial penetration of the biofilm matrix, reduced microbial growth rates, biofilm-induced expression of resistance factors, and other biofilm-induced physiologic changes that decrease susceptibility to antibiotics.
Gastrointestinal Biofilm – The Healthful and the Pathogenic
The human gut is home to approximately 100 trillion microorganisms consisting of unattached planktonic microbes residing in the lumen and sessile biofilm organisms colonizing the mucosa and luminal particulate matter. Among the more important species involved in gastrointestinal biofilm formation are Bacteroides, Bifidobacterium, and Fusobacterium. Fusobacterium species appear to play a key role in formation and maintenance of healthy biofilm by forming coaggregation and coadhesion bridges between early and late bacterial colonizers. However, Fusobacterium, an anaerobic genus, can contribute to pathogenic biofilms because it requires association with an aerobic species in certain environments and hence promotes Streptococcus mutans biofilm in dental plaque leading to caries and Helicobacter pylori biofilm on the gastric mucosa associated with gastric ulcers. Disrupted healthful biofilm permits colonization and biofilm formation by potential pathogens such as Klebsiella pneumoniae, Escherichia coli, and Candida albicans. Potential pathogens residing within biofilms rapidly express genes associated with antimicrobial resistance and are protected from both cellular and humoral immune responses. Successful eradication of pathogen-associated biofilm is critical to elimination of these harmful organisms.
Klaire Laboratories
Many infections that patients are fighting today have some form of biofilm base to them. Antibiotic resistance and biofilms are a growing problem in why some individuals can not conquer these super bug infections. Lyme disease is a classic example of biofilm based problem and the challenge it brings to get it under control. In the last year, I’ve had great success when incorporating specific enzyme based formulas to go after the biofilm component these pathogens present. (Bacterial, viral, candida) Are your doctors addressing this problem?
Dr. J

My husband has MS and is cursed with frequent UTI’s. It is getting more difficult to find a drug that can handle his “complex” E. coli infections . What enzyme formulas would Dr. J recommend for this problem? Thank you, Deirdre Foster
LikeLiked by 1 person
Enzymes I don’t want to mention on here because I don’t want patients to just treat themselves. It needs to me doctor supervised.
LikeLike
Thank you, Dr. Senechal!
Would you and Dr. Tent please consider giving a lecture (to be posted on your YouTube channel) on Lyme Disease? I can’t think of two better Doctors to deliver the goods!
Sincerely,
Aaron
LikeLiked by 1 person
I have some new testing that I’m doing for Lyme. Very complex topic that really no one has under control. Most cases i get better results treating the other co-infections like EBV.
LikeLike
Thanks for the reply, Dr. J. I agree with you on the complexity. As for co-infections, my “regular” (insurance) Doctor doesn’t think my Mycoplasma Pneumoniae is reactivated, as my IgM values are low. But, over the past two years, my IgG values have continued to rise — from the 600s, to the 700s, to the 900s, and now over 1,000. So, in my mind, even if it’s the IgG antibodies, if the number is rising, it would seem to be reactivated. They have no other explanation for why I feel like I was run-over by a Greyhound bus! I’ll call your office and see if I can get a Skype appointment with you. Take care, sir.
LikeLike